No
The Labor & Delivery Experience
Labor is a normal (physiological) process and indicates that the pregnancy is ending. Your healthcare provider will give you an estimated date of birth (EDB) or due date for the baby. Most women carry their baby to 37-40 weeks gestation, or to “term." A baby born at term, without complications, is likely to transition well to life outside your womb.
Babies do not always follow the “rules" of an identified due date, so it is good to be aware of labor signs. Talk with your provider about labor during your prenatal visits and discuss what to do if you think you may be in labor.
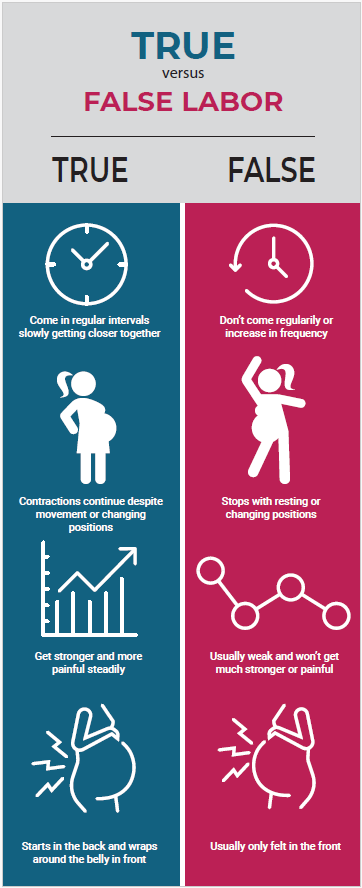
| True Labor Contractions | False Labor Contractions |
| Will become longer, stronger, and closer together | May be regular for a short time, then become irregular |
| Felt in the lower back, radiating to the lower abdomen | Felt in the abdomen above the belly button, or in your back |
| Position changes or walking will make the contractions stronger | Position changes or walking may stop the contractions |
| Comfort measures will not stop or make contractions go away | Comfort measures can stop the contractions |
Adapted from: March of Dimes, American College of Obstetricians and Gynecologists (ACOG)
 True vs False Labor (Printable & Accessible Version)
True vs False Labor (Printable & Accessible Version)
For more information about true versus false labor, visit:
When Your “Water" Breaks…
The bag of waters is the sac of amniotic fluid that your baby lives in within your womb/uterus. This fluid helps to cushion and protect your baby. Sometimes this sac of fluid will break/rupture before the onset of labor, other times it will break during labor.
Anytime during your pregnancy, notify your healthcare provider immediately if you experience vaginal fluid loss.
Pain Management
During labor, your body is working hard. Each woman tolerates and manages labor pain differently, and that is okay! The healthcare team and your partner/support team can help you manage the discomforts or pain of labor and delivery.
During your prenatal appointments, speak with your provider about pain management options that will be available to you and tell them your preferences.
Types of Pain Management for Labor include:
| Non-pharmacological | Pharmacological |
| Light touch, counter pressure | Analgesics (intravenous (IV) medications, inhaled) - Decreases pain sensations
- Increases pain threshold or tolerance
|
| Position changes, movement | |
| Water therapy with warm bath/shower | |
| Relaxation techniques such as mediation, music | Anesthetics (local, spinal, epidural, or general anesthesia) - Blocks pain perception by interrupting nerve impulses to the brain
- Partial or complete loss of sensation which is temporary
|
| Breathing techniques | |
| Aromatherapy | |
Adapted from ACOG
Learn more about pain management during labor and delivery:
Inducing Labor
If your body does not naturally go into labor on its own, or if your healthcare provider decides that there is a medical reason, your labor may be induced. This can be done with medications or other interventions.
If your body is not able to maintain a sufficient pattern for labor progress, your healthcare provider may decide to assist labor with medications or other interventions. This is considered augmentation of your labor.
For additional information about labor induction and augmentation, visit:
Support for Pregnancy and Delivery
As you get ready to have a baby, you should consider attending a childbirth class and developing a birth plan. Your provider, local hospital, and community organizations are good sources of information on upcoming classes. A birth plan will help you communicate your preferences for your birth to your provider and medical team, but your medical needs may make your preferred birth plan unsafe. Based on your needs, and those of your baby, your medical team will aim to meet your desires while using interventions (like medications or a cesarean section) to keep you safe.
Your community wants you to have a happy healthy baby and a safe delivery. A doula may be able to help! A doula is a person who is trained to provide non-medical support around labor and delivery. Some doulas provide support before and after labor and delivery, coming to meet you in your home and may help with things like dishes and food prep when you have a newborn.
To locate a doula provider, please refer to these organizations (e-mail our program to have a new program added to this list):
Methods of Delivery
Each pregnancy, labor, and delivery experience are different. During your prenatal visits, talk with your doctor or midwife about your delivery plan.
Vaginal Delivery
- Occurs when your baby is delivered through your birth canal (vagina)
- Most common method of birthing a baby
- Your healthcare provider may use assistive devices or tools to aid a vaginal delivery
- May not be recommended in certain situations (examples: active genital herpes lesions/infection, previous c-section, fetal malposition or malpresentation, placenta previa or abruption, umbilical cord prolapse)
Cesarean Section (c-section)
- Surgical delivery of your baby through an incision on your abdomen
- Purpose: protect the well-being of the mom and baby
- May be scheduled or unscheduled depending on the circumstances of your pregnancy and labor
For additional information about delivery methods or care for you after your delivery, review these sites and contact your provider if questions:
Skin to Skin Time
Following the delivery of your baby, your healthcare team may place the baby directly to your chest for “skin-to-skin" time. The goal is for you and baby to share this time for at least 60 minutes. Your medical team will encourage this if you and the baby are stable following delivery.
“Skin to skin" time is also known as the Magical, Golden, or Sacred hour. Some refer to this time as kangaroo care. This time is good for both you and the baby as it promotes attachment and breastfeeding, temperature regulation for the baby, and decreases stress.
Your medical team will continue to assess you and your baby during this time. Each birth is different, though skin/skin time with baby is a preferred practice, it is not always possible in every situation.
For additional information about skin-to-skin time with your baby visit:
A new beginning, a new precious life. Enjoy this time and be patient with yourself!