Return to Play
Back in the Game
| Mention of any specific health care facility or organization in the videos reflects an individual’s specific experience and is not intended as an endorsement from this site. |
 |
To minimize the risk of re-injury, it’s recommended that the following criteria are met before a patient begins a Return to Play Progression:
|
As this course has previously emphasized, there must be no same-day Return to Play for an athlete diagnosed with a concussion or an athlete suspected of having a concussion who has not been evaluated by health care professionals. No matter what, once an athlete has returned to baseline, he or she must undertake a multistep progression.
 |
 Courtesy Nebraska Secretary of State’s Office
|
Return to Play ClearanceAccording to the Nebraska Concussion Awareness Act, a licensed health care professional must give written clearance to Return to Play. The law says:"Such student shall not be permitted to participate in any school supervised team athletic activities involving physical exertion, including, but not limited to, practices or games, until the student (i) has been evaluated by a licensed health care professional, (ii) has received written and signed clearance to resume participation in athletic activities from the licensed health care professional, and (iii) has submitted the written and signed clearance to resume participation in athletic activities to the school accompanied by written permission to resume participation from the student’s parent or guardian." |
Clearance to Return to Play LetterThis course recommends being very clear in your letter. Your initial role is to provide clearance for the progression to Return to Play. That is not the same as clearance to return to full activities and competition. You need to set the standards and steps for what the patient is allowed to do at what stage in the progression, based on symptoms and response to treatment, with continual monitoring and assessment.A Clearance to Return to Play letter is not a carte-blanche license for the child to dive immediately full force into all activities. Be clear about what you’re clearing. Example of Nebraska Sports Concussion Network |
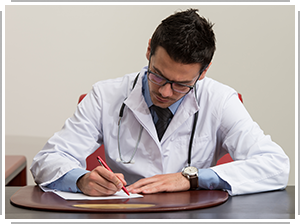 Courtesy ThinkStock: Ibrakovic |
 |
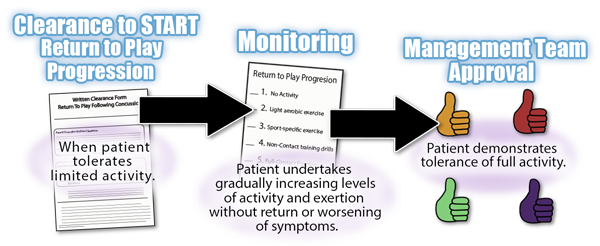
Return to Play ProgressionThis course recommends that an athlete obtains a Clearance to Return to Play letter before undertaking Stage 2 in the Return to Play progression. That is a conservative approach, but conservatism is warranted given the risk of re-injury. If there are no problems along the way, the patient may progress from one step to the next and must complete all steps. The standard for high school is about one step per day. |
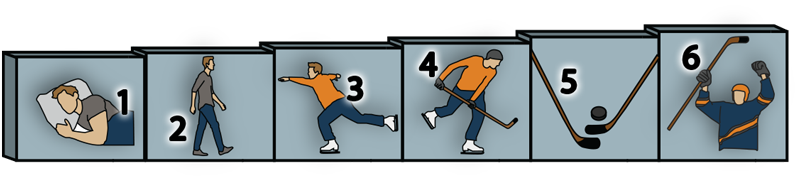 |
GRADUATED RETURN TO PLAY PROGRESSION EXAMPLE |
|
The 4th International Conference on Concussion in Sport Zurich Statement
| Detailed Return to Play Progression ImPACT, UPMC Sports Medicine Concussion Program Guidelines for Post-Concussion Rehabilitation |
Borg Rating of Perceived Exertion Scale Use this scale as a way of measuring physical activity intensity level to help you evaluate a patient’s readiness to Return to Play. |
When the patient has completed the monitored Return to Play Progression, the patient can be given approval for full contact play by a licensed health care professional. In cases where logistics make multiple trips unfeasible, some licensed health care professionals collaborate with the school professionals to provide the needed assessments and documentation.
