Return to Learn
 |
Return to Activity begins with a Return to Learn Progression. Although Return to Learn is the last of the four components of the Nebraska Concussion Awareness Act, it is actually the most important part of the law. It appears last only because it was added as an amendment to the original legislation. (See Module 1.)
For your patient, Return to Learn is of higher priority than Return to Play. The Return to Learn Progression should always precede the Return to Play progression, because the activity required for the return to learning involves less risk than returning to physical activity, especially rigorous athletics. |
TeamworkTo carry out the Return to Learn Progression, you and your patient will need support, because although concussion is a medical diagnosis, concussion management is a team process. Communication is essential to this process.Mutual respect will enhance your communication with school staff, parents, coaches, athletic trainers, and other team members striving to help your patient recover. You need to delineate the medical picture for the team. Working closely with the schools, your team will determine the best course of action together. For more detail about building and working effectively as a management team, consult resources such as Nebraska Department of Education’s Bridging the Gap. It provides responses to intervention that are student-centric, with family, medical, school, and coaches / athletic personnel supporting the process. NDE’s Bridging the Gap |
 |
|
|||||||
Return to Learn Progression
Return to Learn has its own stages. Prior to beginning a Return to Learn Progression, if there is no increase in symptoms, the individual can engage in daily living activities, undertake relaxation exercises, listen to soft music, listen to an audio book, and so on, adding intervals of 20 minutes at a time.The Return to Learn Progression itself should be individualized and gradual. Students may start at any of these steps, depending on the symptoms. It’s up to the team to continually monitor and assess in order to recommend where the student should be at any point.
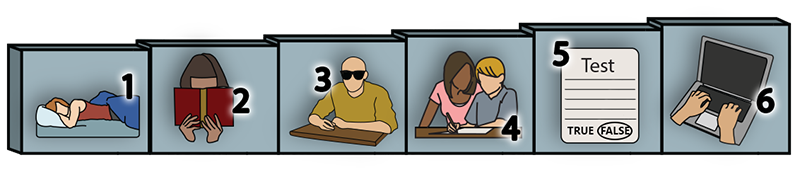 |
RETURN TO LEARN PROGRESSION EXAMPLE |
|
BIRSST Return to Academics Progression
Once the student is back at school part-time, there are various types of adjustments available to help the patient handle various symptoms.
Short Term AdjustmentsA Return to Learn Progression involves short term, temporary adjustments for the student in the classroom. Patients may recover very quickly, but also may be symptomatic for a few months. Short term adjustments may be needed.It will be up to the school to decide which adjustments are necessary and useful for a particular student. For example, you may recommend dark glasses to help the student cope with light sensitivity. But school staff may know that this particular youth is inclined to doze off when wearing dark glasses, so dimming lights would be a better adjustment for him. |
 Courtesy ThinkStock: Padung |
Adjustments may include:
 Courtesy ThinkStock: dkiethr |
Informal adjustments, such as eliminating nonessential parts of assignments so the student can focus on essential material, building rest periods into class, and limiting participation in practices for non-sport activity. |
 Courtesy ThinkStock: NiroDesign |
Formal adjustments, such as being allowed to attend for half days when first back in school to avoid overwork, later start times for the school day, and shorter class periods. |
 Courtesy ThinkStock: dkiethr |
Modifications of curriculum, especially during the first week, such as limiting requirements that involve computer use, extending deadlines, or limiting homework, papers, and tests. |
 Courtesy ThinkStock: MSPhotographic |
Environmental modifications, such as dimming lights, allowing the student to wear earplugs to reduce noise or sunglasses to reduce glare, or eating lunch somewhere darker and quieter than a bright, noisy cafeteria. |
 Courtesy ThinkStock: dkiethr |
Monitoring by medical or academic staff. As discussed earlier, you can help the student self-monitor and know when to limit or quit an activity. |
BIRSST Tips for Teachers
(to help with adjustments for an injured student)
 |
Long Term AccommodationsIn a very small percentage of cases, the patient’s symptoms may be chronic. The concussion management team, in this case led by the school, may determine that the patient may benefit from a Section 504 Education Plan for services, accommodations, or educational aids. In rare cases, more permanent conditions may require an Individualized Educational Plan (IEP). Long term accommodations will be discussed in greater detail in Module 6. |
Section 504 Education Plan

